Artificial Intelligence App for Remote Patient Monitoring A Deep Dive
Artificial intelligence app for remote patient monitoring represents a paradigm shift in healthcare, offering unprecedented opportunities to enhance patient care and streamline clinical workflows. This technology leverages the power of AI to continuously collect, analyze, and interpret patient data from various sources, such as wearable devices and in-home monitoring systems. This provides healthcare professionals with real-time insights into a patient’s health status, enabling proactive interventions and personalized treatment plans.
This exploration delves into the multifaceted aspects of AI-powered remote patient monitoring, from its technological underpinnings and impact on healthcare professionals to its ethical considerations and future potential. We will examine how these applications improve patient outcomes, optimize resource allocation, and transform the delivery of care. Through a detailed analysis of key components, challenges, and future trends, this analysis aims to provide a comprehensive understanding of this rapidly evolving field.
How can an artificial intelligence application for remote patient monitoring enhance the quality of patient care in a real-world clinical setting?
The integration of artificial intelligence (AI) into remote patient monitoring (RPM) represents a paradigm shift in healthcare delivery. By leveraging the power of machine learning and data analytics, AI-powered RPM applications offer the potential to significantly improve patient care, reduce healthcare costs, and enhance the overall efficiency of clinical operations. This technology allows for proactive and personalized interventions, leading to better patient outcomes and a more responsive healthcare system.
Improving Patient Outcomes with AI-Powered RPM
AI-driven RPM systems offer several key advantages that contribute to improved patient outcomes. These systems analyze vast amounts of patient data, including vital signs, activity levels, medication adherence, and patient-reported outcomes, to identify patterns, predict potential health risks, and facilitate timely interventions.
- Reduced Hospital Readmissions: One of the most significant benefits is the potential to reduce hospital readmissions. AI algorithms can detect subtle changes in patient health status that might indicate a worsening condition. For example, an AI system monitoring a patient with heart failure might detect early signs of fluid retention, such as weight gain or increased blood pressure, prompting the system to alert the care team.
This allows for early intervention, such as adjusting medication or providing lifestyle recommendations, to prevent a potential hospitalization. Studies have shown that RPM programs, particularly those incorporating AI, can significantly reduce readmission rates. For instance, a study published in the
-Journal of the American Medical Association* found that RPM programs reduced readmissions by up to 25% in patients with chronic conditions like heart failure and diabetes. - Better Medication Adherence: Medication non-adherence is a major contributor to poor health outcomes. AI-powered RPM systems can improve medication adherence through various means. They can send reminders to patients to take their medications, track medication usage, and identify patients who are not adhering to their prescribed regimens. The AI system can also analyze patient data to understand the reasons for non-adherence, such as side effects or financial constraints, and personalize interventions to address these issues.
For example, if a patient reports experiencing side effects, the system can alert the care team to adjust the medication or provide support. A 2022 study in the
-American Journal of Managed Care* showed that AI-driven interventions increased medication adherence by an average of 15% in patients with chronic obstructive pulmonary disease (COPD). - Early Detection and Intervention: AI algorithms can analyze patient data in real-time to identify early warning signs of disease exacerbations or complications. This allows for prompt intervention before the patient’s condition worsens. For example, an AI system monitoring a patient with diabetes can detect early signs of hyperglycemia or hypoglycemia, allowing the care team to adjust insulin dosages or provide dietary recommendations.
- Personalized Care Plans: AI-powered RPM systems can analyze patient data to create personalized care plans tailored to each patient’s specific needs and preferences. This can include individualized medication regimens, lifestyle recommendations, and educational materials.
- Improved Patient Engagement: AI can enhance patient engagement through interactive platforms that provide patients with personalized feedback, educational resources, and communication tools. This helps patients feel more involved in their care and improves their understanding of their health conditions.
Comparison of AI-Driven RPM vs. Traditional Monitoring
The following table provides a detailed comparison of the functionalities of an AI-driven remote patient monitoring app versus traditional monitoring methods.
| Feature | AI-Driven RPM | Traditional Monitoring | Key Differences |
|---|---|---|---|
| Data Collection | Automated, continuous, and multi-parameter data collection (vital signs, activity, patient-reported outcomes). Integration with wearable devices and sensors. | Manual or intermittent data collection, often relying on patient self-reporting. Limited data points. | AI-driven RPM provides a more comprehensive and continuous stream of data, leading to a more complete picture of the patient’s health. |
| Data Analysis | Real-time analysis using machine learning algorithms to identify patterns, predict risks, and personalize interventions. | Limited analysis, often relying on manual review by healthcare professionals. Reactive rather than proactive. | AI-driven RPM provides faster and more accurate data analysis, enabling proactive interventions and personalized care. |
| Alerting and Notifications | Automated alerts and notifications based on predefined thresholds and predictive algorithms. Prioritization of alerts based on risk. | Manual alerts based on predefined thresholds. Alert prioritization is often reliant on human assessment. | AI-driven RPM offers more timely and targeted alerts, reducing the workload on healthcare professionals and enabling quicker interventions. |
| Intervention and Care Planning | Personalized care plans based on AI-driven insights. Automated recommendations for medication adjustments, lifestyle changes, and follow-up appointments. | Care plans are often based on general guidelines and clinical judgment. Interventions may be delayed due to limited data and analysis. | AI-driven RPM facilitates more personalized and proactive interventions, leading to improved patient outcomes and reduced healthcare costs. |
Ethical Considerations in AI-Powered RPM
The implementation of AI-powered RPM raises several ethical considerations that must be carefully addressed to ensure responsible and equitable use of this technology.Data privacy and security are paramount. The collection, storage, and transmission of sensitive patient data must be protected from unauthorized access and cyber threats. Robust security measures, such as encryption, access controls, and regular security audits, are essential.
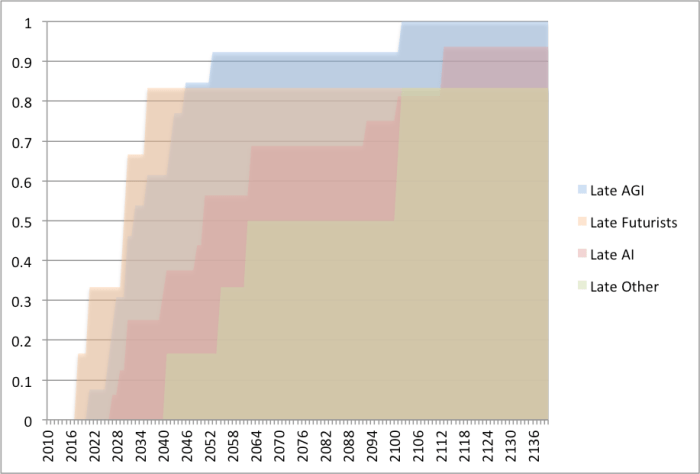
Compliance with data privacy regulations, such as HIPAA in the United States and GDPR in Europe, is mandatory. Data anonymization and de-identification techniques can further protect patient privacy.Algorithmic bias is another critical concern. AI algorithms are trained on data, and if that data reflects existing biases in healthcare, the algorithms may perpetuate or even amplify those biases. This can lead to disparities in care and treatment.
It is crucial to ensure that the data used to train AI algorithms is diverse and representative of the patient population. Regular audits of the algorithms should be conducted to identify and mitigate any biases. Transparency in the design and operation of AI systems is also essential. Patients and healthcare providers should understand how the algorithms work and how they are used to make decisions.Additionally, the use of AI should not replace the human element of care.
Healthcare professionals should remain the primary decision-makers, and AI should be used as a tool to support and augment their clinical judgment. The relationship between the patient and the healthcare provider should be maintained and enhanced, not diminished, by the use of AI. Careful consideration of these ethical factors is crucial for the responsible and effective implementation of AI-powered RPM, ensuring that it benefits all patients and promotes equitable healthcare outcomes.
What are the key technological components that underpin a successful artificial intelligence app for remote patient monitoring, and how do they work together?
The efficacy of an artificial intelligence (AI) application for remote patient monitoring hinges on a complex interplay of sophisticated technological components. These elements must function seamlessly to collect, analyze, and interpret patient data, ultimately providing actionable insights to healthcare providers. The following sections delve into the core technologies and their integrated functionality.
Core Technologies for AI-Powered Remote Patient Monitoring
A successful AI-driven remote patient monitoring system necessitates several core technologies working in concert. These include machine learning algorithms for data analysis, sensor integration for data acquisition, and secure data transmission protocols for privacy and integrity.
- Machine Learning Algorithms: At the heart of the system, machine learning (ML) algorithms are crucial for pattern recognition, anomaly detection, and predictive modeling. These algorithms, trained on vast datasets of patient information, can identify subtle changes in a patient’s condition that might be missed by manual observation. Different types of ML algorithms are employed based on the specific application. For example:
- Supervised Learning: Used to classify data, such as identifying the presence of a disease based on sensor readings (e.g., classifying a patient as “at risk” of a fall based on gait analysis data).
Algorithms like Support Vector Machines (SVMs) and Random Forests are commonly used.
- Unsupervised Learning: Used for data clustering and anomaly detection. Algorithms like K-means clustering can group patients with similar health profiles, and anomaly detection algorithms can flag unusual readings that may indicate a problem.
- Reinforcement Learning: Can be used to optimize treatment plans or alert strategies by learning from patient outcomes.
- Supervised Learning: Used to classify data, such as identifying the presence of a disease based on sensor readings (e.g., classifying a patient as “at risk” of a fall based on gait analysis data).
- Sensor Integration: The system relies on various sensors to collect patient data. These sensors, ranging from wearable devices (e.g., smartwatches, patches) to in-home monitoring systems (e.g., blood pressure monitors, weight scales), capture vital signs, activity levels, and other relevant metrics. The data streams from these sensors must be standardized, cleaned, and integrated into a unified format for analysis.
- Secure Data Transmission Protocols: Protecting patient data is paramount. The system must employ robust security measures to ensure data privacy and integrity. This includes:
- Encryption: Data is encrypted both in transit and at rest using protocols like Transport Layer Security (TLS) and Advanced Encryption Standard (AES).
- Access Controls: Strict access controls limit who can view and modify patient data, adhering to regulations like HIPAA.
- Data Anonymization: Techniques like masking or pseudonymization are used to protect patient identities.
Step-by-Step Data Processing Workflow, Artificial intelligence app for remote patient monitoring
The AI app follows a structured process to collect, analyze, and interpret patient data. This process ensures actionable insights are generated efficiently and accurately.
- Data Collection: Sensors continuously collect patient data, transmitting it to a central server or cloud platform. This data includes vital signs (heart rate, blood pressure, oxygen saturation), activity levels (steps taken, sleep patterns), and other relevant metrics.
- Data Preprocessing: Raw data undergoes preprocessing steps to ensure data quality and reliability. This includes:
- Data Cleaning: Handling missing values, removing outliers, and correcting for sensor errors.
- Data Transformation: Converting data into a suitable format for analysis, such as scaling and normalization.
- Feature Extraction: Relevant features are extracted from the preprocessed data. These features represent key characteristics of the patient’s health status. For example, from heart rate data, features such as average heart rate, heart rate variability, and the presence of any irregularities are extracted.
- Analysis and Interpretation: Machine learning algorithms analyze the extracted features to identify patterns, detect anomalies, and predict potential health risks. This involves:
- Model Training: Machine learning models are trained using historical patient data to recognize patterns and make predictions.
- Model Evaluation: The performance of the trained models is evaluated using various metrics to ensure accuracy and reliability.
- Insight Generation: Based on the analysis, the system generates actionable insights, such as alerts for potential health issues, recommendations for treatment adjustments, or personalized health advice.
- Reporting and Visualization: The insights are presented to healthcare providers through user-friendly dashboards and reports, enabling them to make informed decisions about patient care.
Sensor Integration for Comprehensive Health Assessment
The integration of diverse sensors is essential for providing a comprehensive assessment of a patient’s health. Wearable devices and in-home monitoring systems offer complementary data, painting a holistic picture of the patient’s well-being.Wearable devices, such as smartwatches and fitness trackers, capture real-time data on vital signs, activity levels, and sleep patterns. These devices are non-intrusive and can be worn continuously, providing a continuous stream of data.
For example, a smartwatch can monitor a patient’s heart rate, steps taken, and sleep duration. The data collected from wearable devices can identify potential problems, such as irregular heart rhythms or reduced activity levels.In-home monitoring systems, such as blood pressure monitors and weight scales, provide additional insights into the patient’s health. These systems are often used for patients with chronic conditions, allowing them to monitor their health at home and provide feedback to their healthcare providers.
For instance, a patient with hypertension can regularly measure their blood pressure, and the AI app can track trends and alert the patient or their doctor if the readings are outside the normal range. In-home systems may also include smart scales that track weight changes or devices that monitor blood glucose levels.The combination of data from both wearable and in-home monitoring systems allows for a more complete assessment of a patient’s health.
By integrating these diverse data streams, the AI app can provide a more accurate and comprehensive view of the patient’s health status, leading to improved diagnosis, treatment, and overall patient care.
How does the implementation of an artificial intelligence app for remote patient monitoring change the workflow for healthcare professionals?

The integration of an artificial intelligence (AI) driven remote patient monitoring (RPM) application fundamentally reshapes the operational landscape for healthcare professionals. This technological shift impacts not only the tasks performed but also the distribution of responsibilities and the overall efficiency of patient care delivery. By automating certain aspects of patient monitoring and data analysis, the AI app allows healthcare providers to reallocate their time and resources, focusing on higher-level clinical decision-making and patient interaction.
This transition, however, necessitates a careful consideration of workflow adjustments, training protocols, and strategies to mitigate potential resistance to technological changes.
Shifts in Responsibilities and Tasks
The introduction of an AI-powered RPM system brings about significant changes in the roles and responsibilities of healthcare professionals. Nurses and physicians will experience shifts in their daily routines, primarily due to the automation of data collection and initial analysis. Instead of manually recording vital signs and reviewing patient data, the AI app automates these processes, providing healthcare providers with pre-analyzed information and alerts.
- Nurses: Nurses will likely spend less time on routine data collection and more time on direct patient care, patient education, and addressing alerts generated by the AI system. This includes:
- Responding to AI-generated alerts indicating potential health risks or deviations from the patient’s baseline.
- Providing patients with education and support on using the RPM technology.
- Collaborating with physicians on care plans based on AI-analyzed data.
- Physicians: Physicians will shift their focus towards interpreting the AI-generated insights, making clinical decisions, and managing complex patient cases. Their responsibilities will include:
- Reviewing AI-analyzed data to identify trends, patterns, and potential health issues.
- Developing and adjusting treatment plans based on AI-driven insights.
- Managing patients with chronic conditions using the AI-supported data.
- Other Healthcare Professionals: Other members of the care team, such as pharmacists and therapists, may also experience changes in their workflow. The AI app can facilitate better communication and collaboration by providing a centralized source of patient data, improving the coordination of care.
This transformation allows healthcare providers to operate more efficiently, making more informed decisions, and dedicating more time to patient interaction and complex cases. The AI system acts as an extension of the clinical team, improving their capacity to deliver high-quality care.
Time Savings and Efficiency Gains
The AI-driven RPM app offers substantial time savings and efficiency gains compared to manual patient monitoring processes. These improvements are especially evident in the reduction of time spent on data collection, analysis, and alert management. The following comparative analysis illustrates these differences:
Scenario: Manual Patient Monitoring
- Nurses: Spend a significant amount of time manually collecting vital signs, reviewing patient charts, and manually identifying any deviations from normal ranges. This could take 30-60 minutes per patient per day, depending on the complexity of the case.
- Doctors: Spend time reviewing manually collected data, often requiring additional time to identify and interpret trends. This process can be time-consuming, particularly for a large patient panel.
Scenario: AI-Driven Remote Patient Monitoring
- Nurses: The AI app automates data collection and pre-analyzes the information, immediately highlighting critical changes. Nurses can focus on responding to alerts and providing patient support. This may reduce the time spent on data-related tasks to 5-15 minutes per patient per day.
- Doctors: Physicians receive summarized, pre-analyzed data, which includes alerts, trend analyses, and potential issues, saving them significant time on manual data review. The system provides a focused view of the patient’s health, allowing for quicker and more informed decision-making. The time spent on data review can be reduced by 50% or more.
The efficiency gains are substantial. For example, a study in a cardiology clinic using an AI-powered RPM system demonstrated a 40% reduction in hospital readmissions and a 20% increase in patient engagement, which is consistent with improved efficiency.
Strategies for Training and Addressing Resistance
Implementing an AI-driven RPM system requires comprehensive training and change management strategies to ensure effective adoption and address potential resistance from healthcare staff.
- Training Programs:
- Initial Training: Provide comprehensive training on the AI app’s functionality, including how to use the interface, interpret data, and respond to alerts.
- Hands-on Practice: Offer hands-on practice sessions using simulated patient data to familiarize staff with the system.
- Ongoing Support: Establish ongoing support through workshops, webinars, and online resources to address questions and provide updates.
- Addressing Resistance:
- Communication: Communicate the benefits of the AI app clearly, emphasizing its ability to improve patient care and reduce workload.
- Involvement: Involve healthcare professionals in the implementation process to gather feedback and address concerns.
- Pilot Programs: Conduct pilot programs with selected staff to demonstrate the app’s effectiveness and gain valuable insights.
- Addressing Concerns: Actively address concerns about job security and the impact of the AI app on their roles by highlighting the focus on higher-level clinical decision-making.
By adopting a structured training program and proactively addressing potential resistance, healthcare organizations can facilitate a smooth transition to the AI-driven RPM system, maximizing its potential to improve patient care and enhance the workflow for healthcare professionals.
What are the major challenges and potential pitfalls associated with developing and deploying an artificial intelligence app for remote patient monitoring?
The development and deployment of artificial intelligence (AI) applications for remote patient monitoring (RPM) present a complex landscape. While offering significant potential for improving healthcare, several challenges and pitfalls can hinder their successful implementation. These obstacles range from technical complexities to regulatory hurdles and ethical considerations, demanding careful planning and proactive mitigation strategies.
Obstacles in Development and Implementation
Developing and implementing an AI-powered RPM application is fraught with challenges. Healthcare organizations and developers must navigate numerous obstacles to ensure the app’s effectiveness, safety, and regulatory compliance.
- Data Accuracy and Quality: The performance of any AI model heavily relies on the quality and accuracy of the data it’s trained on. Inaccurate or incomplete data can lead to flawed predictions and potentially harmful clinical decisions. This includes issues like incorrect patient-reported data, faulty sensor readings, and inconsistencies in electronic health records (EHRs).
- Algorithm Bias: AI algorithms can inadvertently perpetuate biases present in the training data. If the data used to train the model does not represent the diversity of the patient population, the algorithm may perform poorly for certain demographic groups. This can lead to disparities in care and reinforce existing health inequalities.
- Data Privacy and Security: Protecting sensitive patient data is paramount. AI-powered RPM applications must adhere to strict data privacy regulations, such as HIPAA in the United States, and implement robust security measures to prevent unauthorized access and data breaches. Failure to do so can result in significant legal and reputational damage.
- Integration with Existing Systems: Seamless integration with existing healthcare systems, including EHRs, is crucial for the successful adoption of AI-powered RPM applications. Interoperability challenges can hinder data exchange, complicate workflows, and limit the app’s utility.
- Regulatory Hurdles: The regulatory landscape for AI in healthcare is evolving. Obtaining the necessary certifications and approvals from regulatory bodies, such as the FDA, can be a time-consuming and costly process. The lack of clear guidelines and standards can further complicate the development and deployment of these applications.
- User Adoption and Training: Healthcare professionals and patients must be trained to effectively use and interpret the results generated by the AI-powered RPM application. Resistance to change, lack of trust in the technology, and inadequate training can hinder user adoption and limit the app’s impact.
- Maintenance and Updates: AI models require ongoing maintenance and updates to ensure their accuracy and relevance over time. This includes retraining the models with new data, addressing performance issues, and adapting to changes in clinical guidelines. Failure to maintain the app can lead to its obsolescence and decreased effectiveness.
Impact of Data Errors
Data errors significantly impact the performance of AI-powered RPM applications, potentially leading to inaccurate diagnoses, inappropriate treatment recommendations, and adverse patient outcomes. Identifying and mitigating these errors is crucial for ensuring the reliability and safety of these systems.
- Common Data Errors: Data errors can manifest in various forms. For instance, incorrect entries of patient vital signs (blood pressure, heart rate) due to manual input errors or sensor malfunctions can skew the AI model’s analysis. Incomplete patient histories, missing medication lists, or inaccurate symptom descriptions further compromise the data.
- Impact on App Performance: These errors directly affect the AI model’s ability to accurately identify patterns, predict risks, and generate personalized recommendations. For example, an AI model trained on faulty blood pressure readings might misclassify a patient’s risk of cardiovascular events, leading to inadequate or inappropriate treatment.
- Minimizing Data Errors: Several strategies can be employed to minimize data errors. Implementing robust data validation procedures, including automated checks for implausible values and inconsistencies, is essential. Regular sensor calibration and maintenance are crucial to ensure the accuracy of data collection. Encouraging patient education and self-reporting best practices can also help improve the quality of patient-reported data. Utilizing data from multiple sources and cross-validating the information can improve the accuracy of the application.
Understanding the Regulatory Landscape
Navigating the regulatory landscape is essential for launching an AI-powered RPM application. Compliance with data privacy laws and obtaining necessary certifications are critical for ensuring patient safety and legal compliance.
- Data Privacy Laws: Healthcare organizations must comply with stringent data privacy regulations. In the United States, the Health Insurance Portability and Accountability Act (HIPAA) sets the standards for protecting sensitive patient health information (PHI). This includes rules regarding data security, patient access, and breach notification. Globally, regulations like the General Data Protection Regulation (GDPR) in Europe impose similar requirements, emphasizing data minimization, purpose limitation, and patient consent.
- HIPAA Compliance: Achieving HIPAA compliance involves implementing physical, technical, and administrative safeguards to protect PHI. This includes encrypting data, restricting access to authorized personnel, and conducting regular risk assessments. Organizations must also have robust breach notification procedures in place to comply with HIPAA’s breach notification rule.
- FDA Regulations and Certifications: Depending on the intended use of the AI-powered RPM application, it may be subject to regulatory oversight by the Food and Drug Administration (FDA). The FDA classifies medical devices based on their risk level, with higher-risk devices requiring more stringent review processes. The FDA’s 510(k) premarket notification process is commonly used for AI-based medical devices. Obtaining FDA clearance or approval can be a lengthy and resource-intensive process.
- Required Certifications: Beyond FDA approval, other certifications may be required. These could include certifications related to data security (e.g., ISO 27001) or specific industry standards. Organizations should consult with legal and regulatory experts to ensure they meet all applicable requirements.
How can an artificial intelligence app for remote patient monitoring be tailored to address the unique needs of different patient populations?
The adaptability of an artificial intelligence (AI) app for remote patient monitoring is crucial for its effectiveness across diverse patient populations. This requires a nuanced approach, acknowledging that the needs and characteristics of individuals with chronic diseases, varying cultural backgrounds, and different levels of technological literacy are vastly different. Successful tailoring involves customization of the app’s functionality, user interface, and data interpretation to maximize patient engagement, improve clinical outcomes, and ensure equitable access to care.
Customization for Chronic Disease Management
AI-powered remote patient monitoring apps can be specifically tailored to support patients with chronic diseases by adjusting their functionality and data interpretation based on the specific disease and the patient’s individual needs. This personalization involves several key aspects.For diabetes management, the app can integrate with continuous glucose monitors (CGMs) and insulin pumps to provide real-time data on blood glucose levels.
The AI algorithms can analyze these data points, along with information on diet, exercise, and medication adherence, to provide personalized recommendations for adjusting insulin dosages, dietary choices, and activity levels. The app can alert patients to potential hyperglycemic or hypoglycemic events and provide guidance on how to manage them. For instance, the app could learn the patient’s typical dietary habits and recommend specific adjustments to their meal plan based on their glucose response to certain foods.
Furthermore, the app can predict future glucose trends, enabling proactive intervention.For heart failure patients, the app can track vital signs like blood pressure, heart rate, and weight, which are critical indicators of fluid overload. The AI can analyze these data, combined with information on medication adherence and symptoms reported by the patient (e.g., shortness of breath, swelling), to detect early signs of decompensation.
The app can then alert the patient and their care team to the need for medical intervention, potentially preventing hospitalizations. The AI could learn the patient’s baseline vital signs and flag deviations that suggest worsening heart failure. For example, a sudden increase in weight combined with elevated blood pressure could trigger an alert to the patient’s healthcare provider.The app’s algorithms can be trained on disease-specific datasets to improve accuracy in predicting adverse events.
The app can also integrate with electronic health records (EHRs) to provide a comprehensive view of the patient’s medical history, medication list, and lab results, allowing for more informed decision-making by both the patient and the care team.
Personalizing the User Interface and Data Visualizations
Effective patient engagement and adherence to remote monitoring programs depend significantly on a user-friendly and personalized interface. Customization of the user interface and data visualizations plays a vital role in improving patient engagement and adherence to the monitoring program.The user interface should be adaptable to the patient’s technological literacy. For patients with limited digital skills, a simplified interface with large fonts, clear instructions, and minimal navigation complexity is crucial.
For more tech-savvy patients, a more feature-rich interface with advanced data visualizations and customization options might be preferable.Data visualizations should be tailored to the patient’s preferences and understanding. For example, patients might prefer to see their blood pressure readings presented as a simple graph over time, while others might prefer a more detailed dashboard with color-coded alerts and trend lines.
The app can offer different visual representations of the data, such as bar graphs, line graphs, or interactive dashboards, allowing patients to choose the format that best suits their needs.The app should also provide personalized feedback and educational content. The AI can analyze the patient’s data and provide tailored recommendations for improving their health. This might include reminders to take medication, suggestions for dietary changes, or encouragement to exercise.
The app can also provide educational resources, such as articles and videos, that are relevant to the patient’s specific condition and needs. The app can be designed to deliver information in small, digestible chunks to avoid overwhelming the user. Push notifications can be customized to deliver timely reminders and alerts, encouraging patients to actively engage with their health data.
Incorporating Cultural Sensitivity and Language Accessibility
Ensuring the inclusivity and effectiveness of an AI-powered remote patient monitoring app requires careful consideration of cultural sensitivity and language accessibility. This involves several key strategies.The app’s design should be culturally sensitive, avoiding potentially offensive or culturally inappropriate imagery, language, or symbols. The user interface should be localized to reflect the cultural norms and values of the target patient populations.
This includes using culturally appropriate images and icons, as well as adapting the tone and style of the communication. For instance, in some cultures, direct communication styles may be considered impolite; the app’s messaging should be adjusted accordingly.Language accessibility is paramount. The app should be available in multiple languages, with accurate translations of all text and audio content. The app should support multiple dialects and regional variations of languages to ensure clarity and comprehension.
Furthermore, the app should provide options for audio narration and voice input to accommodate patients with visual impairments or those who prefer to interact with the app using voice commands.The app’s content should be culturally relevant. Educational materials and health information should be adapted to reflect the specific health needs and cultural beliefs of the target populations. For example, dietary recommendations should consider culturally specific food preferences and availability.
The app should also provide access to culturally competent healthcare providers, allowing patients to connect with clinicians who understand their cultural background and can provide appropriate care.
What are the cost implications of adopting an artificial intelligence app for remote patient monitoring, and how can the return on investment be maximized?
The adoption of an artificial intelligence (AI) app for remote patient monitoring (RPM) presents a complex interplay of costs and potential returns. A thorough understanding of these financial aspects is crucial for healthcare providers aiming to integrate AI-driven RPM systems effectively. Strategic planning, including securing funding and maximizing return on investment (ROI), is paramount for successful implementation and long-term sustainability.
Costs Associated with AI-Driven RPM Systems
Implementing an AI-driven RPM system involves a multifaceted cost structure. These expenses can be broadly categorized into development, implementation, and ongoing maintenance. Careful consideration of these elements is essential for accurate budgeting and financial planning.
- Development Costs: These include the initial investment in the AI algorithms and the software platform. This also covers the costs of data scientists, software engineers, and machine learning specialists involved in developing and training the AI models. The complexity of the algorithms, the volume and variety of data used for training, and the desired level of accuracy all influence these costs.
The development phase can be time-consuming, requiring significant upfront investment.
- Hardware Costs: This category encompasses the purchase or lease of wearable sensors, monitoring devices (e.g., blood pressure monitors, pulse oximeters), and data transmission infrastructure (e.g., cellular gateways, secure Wi-Fi). The choice of hardware will depend on the specific medical conditions being monitored and the desired level of patient comfort and data accuracy. Costs can vary widely depending on the sophistication and functionality of the devices.
- Software and Licensing Fees: The AI app itself, along with its associated software infrastructure (e.g., cloud storage, data analytics platforms), will incur licensing fees or subscription costs. Ongoing software maintenance, updates, and security measures also contribute to these expenses. The cost structure can depend on factors like the number of users, data storage requirements, and the level of support provided by the vendor.
- Implementation and Integration Costs: This includes the expenses associated with integrating the RPM system with existing electronic health records (EHRs), training healthcare staff on how to use the system, and providing patient education on the use of the devices and app. Effective integration is vital for the seamless flow of data and efficient clinical workflows. The complexity of the integration process can significantly impact costs.
- Staffing and Training Costs: Healthcare providers need to factor in the costs of training staff on the new system and potentially hiring new personnel to manage the RPM program. This can include clinical staff to monitor patient data, IT staff to maintain the system, and data analysts to interpret the data and provide insights.
- Data Management and Security Costs: Ensuring data privacy and security is critical. This involves implementing robust security measures, complying with regulations such as HIPAA, and potentially hiring cybersecurity experts. Data storage, backup, and recovery costs also contribute to this category.
- Maintenance and Support Costs: Ongoing maintenance includes hardware repairs and replacements, software updates, and technical support. These costs are essential to ensure the continuous operation and reliability of the RPM system.
Potential Financial Benefits and ROI
The financial benefits of AI-driven RPM systems can be substantial, often leading to a positive ROI. These benefits can accrue through various mechanisms, including reduced healthcare utilization and improved operational efficiency.
- Reduced Hospitalizations: By enabling early detection of potential health issues, RPM can help prevent hospital admissions. This is particularly relevant for chronic conditions such as heart failure, diabetes, and COPD. For instance, studies have shown that RPM programs for heart failure patients can reduce hospital readmissions by 20-30%.
- Fewer Emergency Room Visits: Early intervention facilitated by RPM can reduce the need for emergency room visits. This translates into cost savings for both patients and healthcare providers.
- Reduced Length of Stay: RPM can support earlier discharge from the hospital, freeing up beds and reducing the length of hospital stays.
- Improved Medication Adherence: AI-driven systems can monitor medication adherence and provide reminders, leading to improved patient outcomes and reduced costs associated with non-adherence.
- Enhanced Operational Efficiency: AI can automate data analysis, streamline workflows, and free up clinicians’ time. For example, AI algorithms can automatically flag patients at high risk, allowing clinicians to focus on those who need immediate attention.
- Reduced Physician Workload: Automating data analysis and providing insights can reduce the time physicians spend reviewing patient data, allowing them to focus on patient care.
- Increased Patient Satisfaction: Patients often report increased satisfaction with RPM programs, leading to improved outcomes and reduced costs associated with adverse events.
- Potential for Pay-for-Performance Models: Healthcare providers can leverage RPM data to participate in pay-for-performance models, where reimbursement is tied to quality metrics and outcomes.
Strategic Plan for Funding and Partnerships
Securing funding and establishing strategic partnerships are critical steps in deploying and maintaining an AI-driven RPM app. A well-defined plan, including various funding sources and collaborations, can facilitate the successful implementation and long-term sustainability of the system.A multi-pronged approach to funding is recommended. Healthcare providers can explore grants from government agencies, such as the National Institutes of Health (NIH) or the Centers for Medicare & Medicaid Services (CMS).
Venture capital and private equity firms are increasingly investing in healthcare technology, and these sources can provide significant capital. Strategic partnerships with technology companies and device manufacturers can also provide financial support and expertise.Building strong partnerships is equally important. Collaborating with technology companies can provide access to advanced AI algorithms and software platforms. Partnerships with device manufacturers can provide access to the latest wearable sensors and monitoring devices.
Establishing relationships with payers (insurance companies) can help secure reimbursement for RPM services. Patient advocacy groups can provide valuable insights into patient needs and preferences. These partnerships can help ensure the long-term success of the RPM program.
How does the integration of an artificial intelligence app for remote patient monitoring impact patient-provider communication and collaboration?
The integration of an artificial intelligence (AI) app for remote patient monitoring (RPM) fundamentally reshapes the dynamics of patient-provider communication and collaboration. This transformation stems from the app’s ability to facilitate continuous data collection, provide timely alerts, and offer secure channels for information exchange. The shift moves beyond episodic interactions to a more proactive and data-driven approach, fostering a stronger partnership between patients and their healthcare providers.
Facilitating Enhanced Communication
The AI-powered RPM app acts as a central hub for communication, leveraging various features to enhance patient-provider interactions. These features move beyond traditional methods, offering more efficient and effective ways to exchange information and manage care.
- Alerts and Notifications: The app generates real-time alerts and notifications based on predefined parameters and AI-driven analysis of patient data. For example, if a patient’s blood pressure exceeds a critical threshold, the system immediately notifies both the patient and the healthcare provider. This proactive approach allows for timely interventions, preventing potential complications and improving patient outcomes.
- Secure Messaging: Secure messaging features enable confidential communication between patients and providers. Patients can securely send messages, share updates on their symptoms, and ask questions. Providers can respond promptly, provide guidance, and address concerns remotely. This eliminates the need for phone calls or emails that might be less secure and ensures a documented record of the communication.
- Data Visualization: The app presents patient data in an easily understandable format, using charts, graphs, and trends. This visual representation of data helps both patients and providers to quickly grasp the patient’s health status, identify patterns, and track progress over time. The visualization tools also make it easier for patients to actively participate in their care.
- Automated Reporting: The AI app automates the generation of reports summarizing the patient’s health data, medication adherence, and other relevant information. These reports are easily accessible to both patients and providers.
Comparative Analysis of Communication Strategies
The effectiveness of different communication strategies in improving patient-provider relationships varies based on the features used and their implementation. The following table provides a comparative analysis:
| Communication Strategy | Features | Effectiveness in Improving Patient-Provider Relationships |
|---|---|---|
| Traditional Communication | Phone calls, in-person appointments, emails | Limited by time constraints, lack of real-time data, and potential for information gaps. Can be effective for specific issues but are generally reactive. |
| AI-Powered RPM with Basic Features | Alerts, basic messaging, data logging | Improves responsiveness, offers more data, and facilitates proactive intervention. The patient’s involvement increases, but the depth of communication might still be limited. |
| AI-Powered RPM with Advanced Features | Alerts, secure messaging, data visualization, automated reporting, integration with patient portals | Highest effectiveness due to real-time data analysis, proactive alerts, streamlined communication, and increased patient engagement. The app enhances the partnership by offering a complete picture of the patient’s health, allowing for informed decisions. |
Utilizing AI Data for Collaborative Care
The data generated by the AI app is a valuable resource for fostering shared decision-making and enhancing the overall collaborative care experience. Healthcare providers can use the app’s data analysis and visualization capabilities to enhance patient care.
- Shared Decision-Making: The data provides a common ground for discussions about treatment options, lifestyle modifications, and medication adjustments. For instance, if the app reveals that a patient’s blood glucose levels are consistently elevated after meals, the provider can use this information to discuss dietary changes or medication adjustments.
- Enhanced Patient Education: The app’s reports and visualizations can be used to educate patients about their health conditions and the impact of their behaviors on their health. This improved understanding empowers patients to make informed decisions about their care.
- Improved Medication Adherence: By tracking medication adherence through the app, providers can identify patients who are struggling to follow their prescribed regimens. This information allows for timely interventions, such as reminders, counseling, or adjustments to the medication schedule, to improve adherence and treatment outcomes.
- Personalized Care Plans: The data from the AI app can be used to tailor care plans to the individual needs of each patient. For example, if a patient’s activity levels are consistently low, the provider can recommend specific exercises or lifestyle modifications to increase physical activity.
What are the future trends and advancements expected in the field of artificial intelligence apps for remote patient monitoring?
The field of artificial intelligence (AI) in remote patient monitoring (RPM) is poised for rapid advancement, driven by emerging technologies that promise to revolutionize healthcare delivery. These innovations aim to enhance patient care, optimize clinical workflows, and improve the efficiency of healthcare systems. This section explores key future trends, including advanced machine learning algorithms, predictive analytics, and the integration of virtual assistants, along with their potential impact and associated ethical considerations.
Emerging Technologies and Their Impact
Several technological advancements are expected to reshape the landscape of AI-powered RPM. These advancements will likely lead to more personalized, proactive, and efficient healthcare.
- Advanced Machine Learning Algorithms: Deep learning, a subset of machine learning, will become increasingly prevalent. These algorithms, utilizing neural networks with multiple layers, can analyze vast datasets of patient data, including vital signs, lab results, and lifestyle information, to identify complex patterns and make more accurate predictions. This allows for early detection of potential health issues. For example, deep learning models can analyze electrocardiogram (ECG) data to predict the risk of cardiac events with higher accuracy than traditional methods.
- Predictive Analytics: Predictive analytics will move beyond simple risk stratification to provide personalized risk scores and forecasts. These systems will leverage machine learning models to forecast disease progression, predict hospital readmissions, and anticipate adverse events. A real-world example is the use of predictive analytics in diabetes management, where algorithms analyze glucose readings, insulin dosage, and activity levels to predict future glucose levels and recommend personalized interventions.
- Integration of Virtual Assistants: Virtual assistants, powered by natural language processing (NLP), will play a more significant role in patient interaction and care coordination. These assistants can provide medication reminders, answer patient questions, and even facilitate telehealth consultations. Virtual assistants can also streamline communication between patients and healthcare providers by automatically generating summaries of patient interactions and relaying relevant information to the care team.
An example of this integration is the use of virtual assistants to monitor patients with chronic obstructive pulmonary disease (COPD), providing real-time feedback on their breathing patterns and alerting clinicians to potential exacerbations.
- Advanced Sensor Technology: The development of miniaturized and wearable sensors will continue. These sensors will collect a wider range of physiological data, including sleep patterns, activity levels, and even emotional states. This will provide a more comprehensive view of a patient’s health and enable more proactive interventions. For example, wearable sensors can detect subtle changes in gait that may indicate the onset of Parkinson’s disease, allowing for early diagnosis and treatment.
Transforming Healthcare Delivery
The integration of these technologies has the potential to transform healthcare delivery in several key ways.
- Improved Patient Outcomes: By enabling early detection and intervention, AI-powered RPM can lead to improved patient outcomes. Predictive analytics can help prevent complications, reduce hospital readmissions, and improve overall quality of life.
- Streamlined Clinical Workflows: AI can automate routine tasks, such as data analysis and report generation, freeing up healthcare professionals to focus on patient care. Virtual assistants can handle administrative tasks, such as scheduling appointments and answering patient inquiries, reducing the workload on clinicians.
- Personalized Care: AI algorithms can analyze individual patient data to provide personalized treatment plans and recommendations. This allows healthcare providers to tailor interventions to the specific needs of each patient, leading to more effective care.
- Increased Accessibility: RPM can improve access to healthcare, particularly for patients in remote areas or those with limited mobility. Telehealth consultations and remote monitoring can reduce the need for in-person visits, making healthcare more convenient and accessible.
Ethical Implications and Preparation
As AI-powered RPM systems become more sophisticated, several ethical implications must be addressed. Preparing for these challenges is crucial to ensure responsible and equitable implementation.
- Data Privacy and Security: Protecting patient data is paramount. Robust security measures, including encryption and access controls, are essential to prevent unauthorized access and data breaches. Compliance with data privacy regulations, such as HIPAA, is crucial.
- Algorithmic Bias: AI algorithms can perpetuate biases present in the training data, leading to unfair or inaccurate predictions for certain patient populations. Careful attention must be paid to the diversity and representativeness of the data used to train these algorithms. Regular audits and bias mitigation strategies are necessary.
- Transparency and Explainability: It is important to understand how AI algorithms arrive at their conclusions. Explainable AI (XAI) techniques can help make these algorithms more transparent and allow healthcare professionals to understand the rationale behind the recommendations.
- Patient Autonomy: Patients must be informed about how their data is being used and have the right to control their health information. Informed consent and patient education are essential to maintain trust and ensure patient autonomy.
How can the performance of an artificial intelligence app for remote patient monitoring be continuously evaluated and improved over time?
Continuous evaluation and improvement are crucial for the long-term success and efficacy of any AI-driven remote patient monitoring (RPM) application. This iterative process ensures the app remains accurate, reliable, and relevant to the evolving needs of patients and healthcare providers. It involves a multi-faceted approach, incorporating rigorous data analysis, user feedback, and algorithm refinement to optimize performance and maximize clinical impact.
Measuring the App’s Effectiveness
Effectiveness measurement relies on a combination of quantitative and qualitative methods to assess the AI app’s impact. This includes the establishment of key performance indicators (KPIs) and the collection of patient satisfaction metrics.The following methods are utilized to quantify the app’s performance:
- Key Performance Indicators (KPIs): KPIs are crucial for objectively measuring the app’s success. These metrics provide a quantifiable way to track performance over time. Examples of KPIs include:
- Accuracy of Predictions: This is measured by comparing the AI’s predictions (e.g., risk scores, alerts for adverse events) with actual clinical outcomes. Metrics like precision, recall, F1-score, and area under the receiver operating characteristic curve (AUC-ROC) are used to assess the accuracy.
For instance, if an AI app predicts hospital readmission risk, the accuracy can be determined by comparing the prediction with actual readmission events.
- Alert Sensitivity and Specificity: The app’s ability to correctly identify true positives (sensitivity) and true negatives (specificity) is crucial. A balance must be struck to avoid excessive false alarms (reducing provider trust) and missed critical events (harming patients).
- Time to Intervention: The time elapsed between an alert being triggered and a healthcare provider taking action. A shorter time indicates improved responsiveness.
- Reduction in Hospital Readmissions: Track the percentage reduction in hospital readmissions for patients using the app compared to a control group.
- Improvement in Patient Adherence: Monitor medication adherence, lifestyle changes, and other behaviors related to patient health.
- Data Completeness: The percentage of data points successfully collected and transmitted.
- Accuracy of Predictions: This is measured by comparing the AI’s predictions (e.g., risk scores, alerts for adverse events) with actual clinical outcomes. Metrics like precision, recall, F1-score, and area under the receiver operating characteristic curve (AUC-ROC) are used to assess the accuracy.
- Patient Satisfaction Metrics: Patient feedback is vital for assessing the app’s usability and impact on patient experience. This involves collecting data through:
- Patient Surveys: Regularly administered surveys using validated instruments (e.g., the Patient Satisfaction Questionnaire) to gauge satisfaction with the app’s ease of use, helpfulness, and perceived impact on their health.
- Focus Groups and Interviews: Qualitative data collection to gather in-depth insights into patient experiences, identify areas for improvement, and understand patient preferences.
- Net Promoter Score (NPS): Measures the likelihood of patients recommending the app to others.
Designing a Framework for Regular Audits and Reviews
Regular audits and reviews are essential for identifying areas for improvement within the AI app. A structured framework ensures a systematic approach to performance evaluation and algorithm refinement.A comprehensive audit and review framework should include the following components:
- Scheduled Audits: Regular audits, such as quarterly or bi-annual reviews, should be established to assess the app’s performance against predefined KPIs.
- Data Analysis:
- Data Validation: Verify the integrity and accuracy of the data used by the AI model.
- Statistical Analysis: Perform statistical analyses to identify trends, patterns, and anomalies in the data.
- Cohort Analysis: Compare the performance of the app across different patient subgroups to identify potential biases or areas where the app’s performance may vary.
- Algorithm Performance Review:
- Model Drift Detection: Continuously monitor the AI model for performance degradation over time (model drift). This can occur due to changes in patient populations, clinical practices, or data patterns.
- Retraining and Refinement: Retrain the AI model periodically using updated data to ensure continued accuracy and relevance.
- User Feedback Integration:
- Feedback Mechanisms: Establish clear mechanisms for collecting feedback from healthcare providers and patients (e.g., in-app feedback forms, dedicated support channels).
- Feedback Analysis: Analyze user feedback to identify usability issues, feature requests, and areas where the app could be improved.
- Documentation and Reporting:
- Comprehensive Documentation: Maintain detailed documentation of all audit findings, algorithm updates, and performance improvements.
- Regular Reporting: Generate regular reports summarizing the app’s performance, identifying areas for improvement, and tracking progress over time.
Utilizing User Feedback, Clinical Data Analysis, and Algorithm Updates
Refining the AI app’s performance involves a cyclical process of analyzing data, incorporating user feedback, and updating the underlying algorithms. This ensures continuous improvement and adaptation to evolving clinical needs.The following steps are critical for refining the app:
- User Feedback Integration: Actively solicit and analyze feedback from both patients and healthcare providers. This includes:
- Usability Testing: Conduct regular usability testing sessions to identify and address issues related to the app’s user interface (UI) and user experience (UX).
- Feature Prioritization: Prioritize feature requests based on their potential impact on patient care and user satisfaction.
- Clinical Data Analysis: Analyze clinical data collected through the app to identify patterns, trends, and opportunities for improvement. This includes:
- Data Mining: Use data mining techniques to identify new risk factors, improve prediction accuracy, and personalize patient care.
- Anomaly Detection: Implement anomaly detection algorithms to identify unusual patterns in patient data that may indicate a potential health issue.
- Algorithm Updates: Periodically update the AI algorithms based on new data, clinical insights, and user feedback. This includes:
- Model Retraining: Retrain the AI model with new data to improve its accuracy and generalizability.
- Algorithm Optimization: Optimize the AI algorithms to improve their performance, efficiency, and interpretability.
- Version Control: Implement a robust version control system to track changes to the AI model and ensure that updates are properly tested and validated before deployment.
- Iterative Improvement Cycle: Implement a continuous feedback loop where findings from data analysis and user feedback are used to inform algorithm updates, which in turn lead to improved clinical outcomes and user satisfaction. This cycle is critical for sustained success.
Closing Notes
In conclusion, the integration of an artificial intelligence app for remote patient monitoring heralds a new era in healthcare, marked by enhanced patient outcomes, improved efficiency, and more personalized care. While challenges such as data privacy and algorithm bias must be addressed, the potential benefits are vast. By embracing innovation and adapting to the evolving landscape, healthcare providers can harness the full power of AI to transform the delivery of care and create a healthier future for all.
Answers to Common Questions
What types of data can an AI-powered remote patient monitoring app collect?
These apps can collect a wide range of data, including vital signs (heart rate, blood pressure, temperature), activity levels, sleep patterns, medication adherence, and patient-reported outcomes (symptoms, pain levels).
How is patient data protected within these applications?
Data privacy is a priority. These apps employ robust security measures, including encryption, secure data transmission protocols, and compliance with regulations like HIPAA to protect patient information.
What is the role of healthcare providers in using these AI apps?
Healthcare providers use these apps to monitor patients remotely, review alerts and insights generated by the AI, communicate with patients, and make informed decisions about their care. The app assists, but providers retain clinical judgment.
Are these apps suitable for all patient populations?
While the technology is adaptable, the suitability depends on individual needs and health conditions. Customization and cultural sensitivity are key to ensuring inclusivity and effectiveness for diverse patient groups.
How can I find out if my healthcare provider uses an AI-powered remote patient monitoring app?
Inquire directly with your healthcare provider. Many providers are now integrating these technologies, and they can inform you about their specific practices.